A single damaged cystoscope resulted in 11 patients presenting with Pseudomonas aeruginosa urinary tract infections over a span of nine months.
The incidence of urinary tract infections after flexible cystoscopy ranges from 2 percent to 21.2 percent, according to various studies. But cystoscopy-related outbreaks have been scarcely reported, so “the risk of patient contamination through cystoscopy is poorly known.”
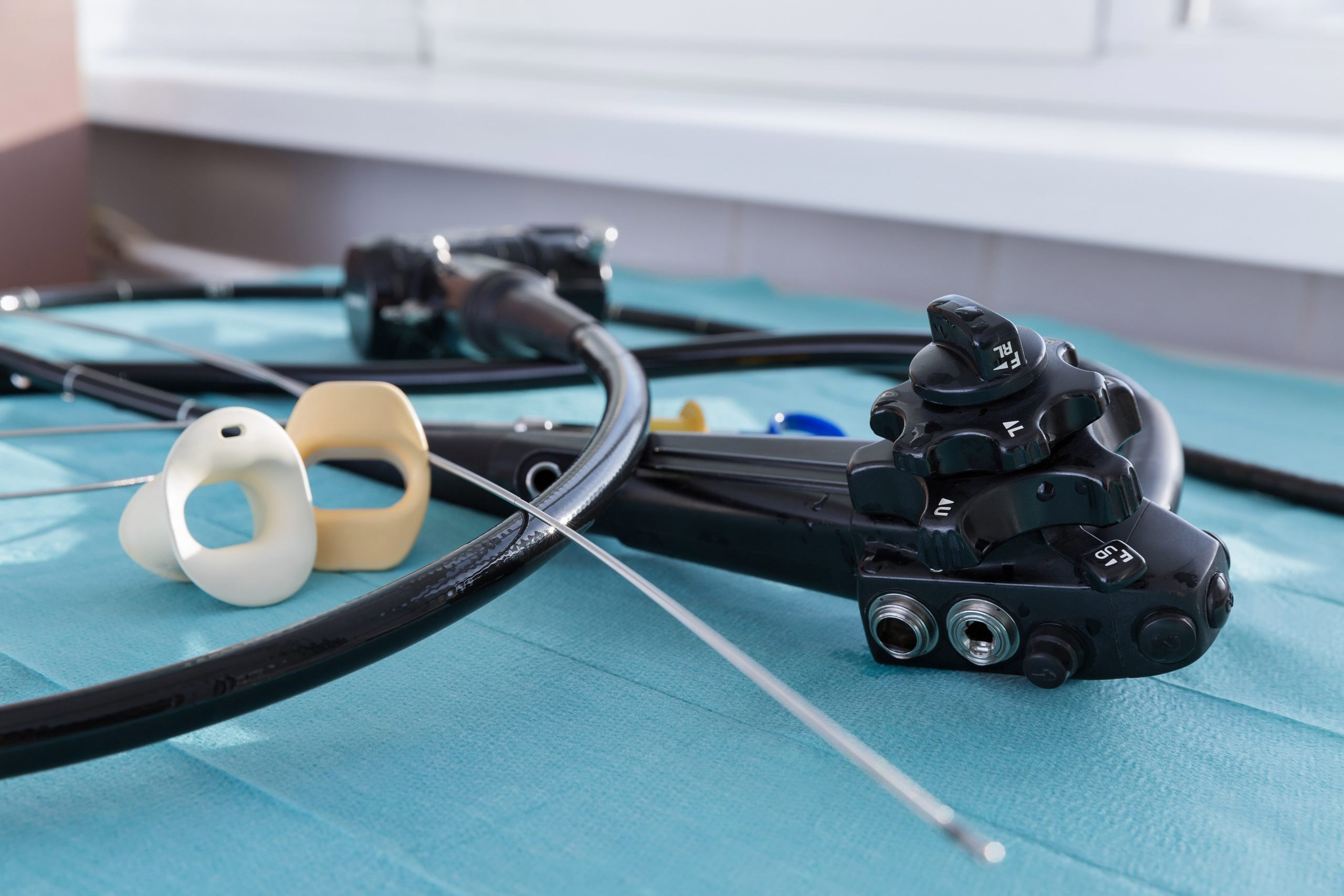
The research, presented in the American Journal of Infection Control, examines an outbreak from several years earlier that followed outpatient flexible cystoscopies. The four reusable cystoscopes used in the institution’s urology consultation would be hand-cleaned and disinfected after each use according to national recommendations.
Microbiological controls were performed at least annually and before reuse after a scope received maintenance. Between July 7, 2015, and May 31, 2016, 389 patients underwent cystoscopies, including 104 who were examined using “cystoscopy number 419.” Every Pseudomonas aeruginosa urinary tract infection could be traced back to it. Three other cystoscopes were used on the remaining 284 patients with no documented infections.
On July 1, 2016, “cystoscope number 419” was sampled and two types of Pseudomonas aeruginosa were identified. It was returned to its manufacturer where it was found to have a channel scratch. The infection-causing bacteria was “probably in biofilm attached on to the channel scratch, which allowed it to resist disinfectants,” according to the researchers.
This is common in other areas of endoscopy, and several outbreaks following bronchoscopy have been “associated with the use of a damaged device, inadequate disinfection, and manufacturing defect.”
The rate of Pseudomonas aeruginosa urinary tract infection caused by the contaminated cystoscope exceeded 10 percent, but the others assume the true number to be higher because of the difficulty to follow up with outpatients. Additionally, benign infections such as UTIs are often untreated.
“This situation underlines the interest to record every cystoscopy procedure and to perform a medical feedback for urinary or infectious symptoms in the month after cystoscopy for inpatients and outpatients,” the article reads.
The authors conclude: “The example of this outbreak urges us not to trivialize UTI occurring after an elective cystoscopy. Patients should be advised to signal the occurrence of urologic symptoms after urologic exploration.”