As researchers continue to examine best practices related to bronchoscopy during the global pandemic, a study from the University of Florida questions whether mandated COVID-19 testing of asymptomatic patients before procedures makes a difference in protecting healthcare workers.
A recent research letter in CHEST written by Drs. Hawazin K. Abbas, Bashar N. Alzghoul and others says that mandatory pre-procedural COVID-19 testing for patients does not necessarily decrease the rate of infection among medical staffers.
They suggest that the absence of mandated testing in advance of procedures may not result in a higher risk of symptomatic SARS-CoV-2 transmission. Patient testing costs both time and money and can even force delays in needed procedures.
“Not mandating testing can decrease the burden on the healthcare system and patients,” the authors write.
The authors made these conclusions after a retrospective analysis of COVID-19 case numbers among healthcare staff at the University of Florida between March 2020 and February 2021.
Florida had high community transmission, with a test positivity rate of 8.5 percent during the study period, so an increased risk of contracting the virus during aerosol-generating procedures such as bronchoscopy would be expected, the authors write. Yet, no bronch suite staff members at the University of Florida, Gainesville, had a workplace-related diagnosis of COVID-19.
Throughout the pandemic, the university screened all patients and visitors for symptoms and asked about recent travel history and possible exposure to COVID-positive patients. But asymptomatic patients were not COVID tested before their bronchoscopy procedures.
Procedure observers were limited, staff was reduced to a core team, and patients were required to wear masks in the waiting room, bronchoscopy suite, and recovery areas.
Also, personnel in the procedure area were required to wear personal protective equipment (PPE) such as disposable gowns, gloves, face shields, and surgical masks. A N95 mask or other respiratory protective device was required during the procedure.
There were 664 outpatient bronchoscopies performed during the study period. A total of four bronchoscopy staff members received COVID-19 nasal testing nine times, and there were no COVID-19 infections among them, the authors write.
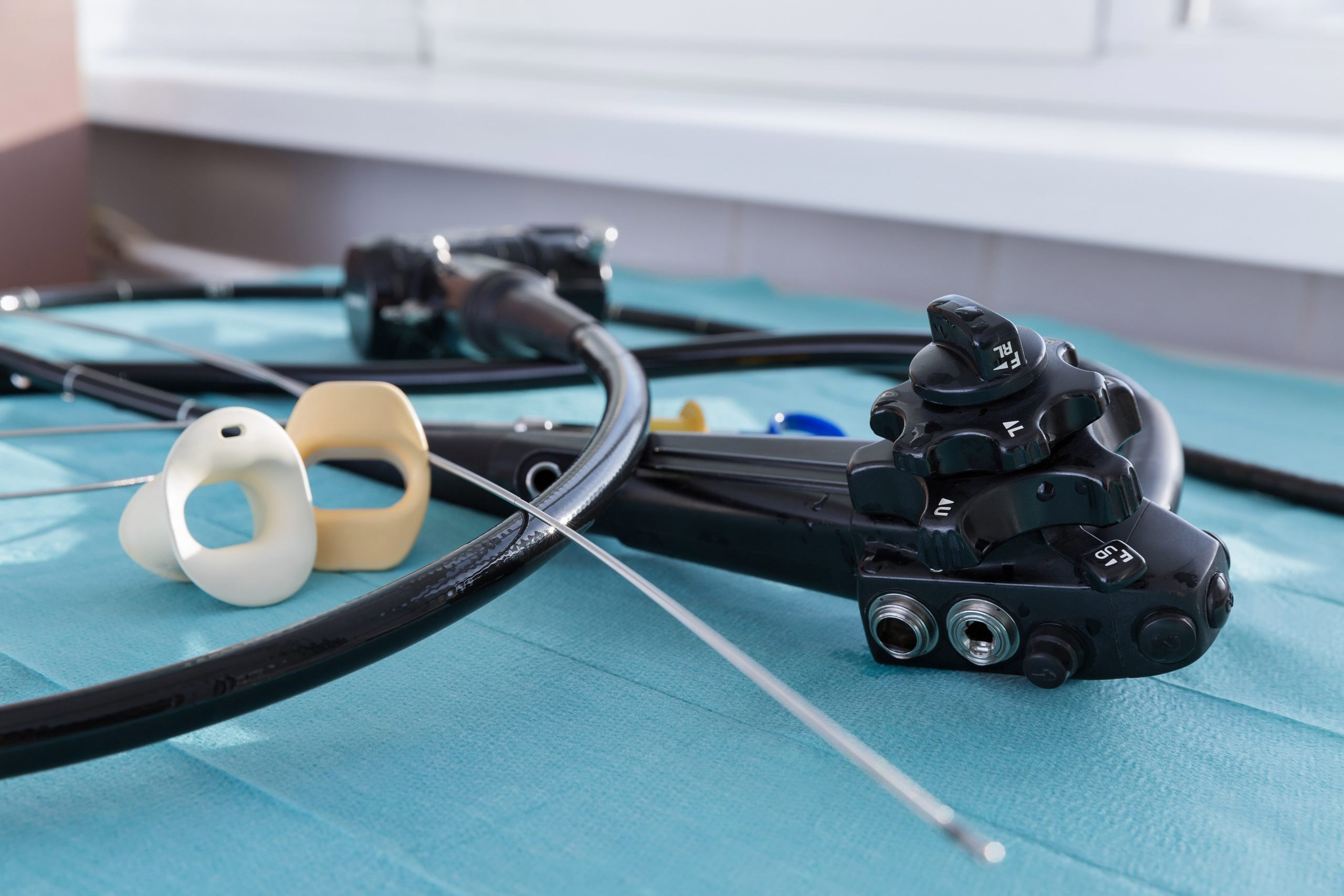
At the start of the pandemic, a variety of medical societies, including the American Society of Bronchology and Interventional Pulmonology, the American College of Chest Physicians, and other specialty groups published guidelines calling for reducing bronchoscopies to only the most necessary and for strict use of PPE. Some recommended single-use bronchoscopes whenever possible, to avoid the risk of cross-contamination.
Early in the pandemic, bronchoscopies effectively came to a halt. They restarted in the weeks and months that followed under careful restrictions.
The authors of the University of Florida research conclude that additional study is needed to see if those results are replicated elsewhere and to identify best practices for surgical procedures going forward.
Currently, full PPE and vaccinations, are the best measures available to protect healthcare workers against COVID-19, they write.