Hospital-acquired infections (HAIs) have been on the rise, but many industry experts agree that education is the most powerful resource for ridding healthcare facilities of dangerous microbes.
Making sure that C-suite executives and decision-makers are well informed about cleaning products and their purposes can help keep infections at bay, according to a post in Healthcare Purchasing News (HPN).
One problem is that environmental services teams do not always have the tools they need, said Dr. Mark Stibich, co-founder of Xenex Disinfection Services, in an interview with HPN.
“Harmful pathogens remain on commonly touched surfaces, even after the best liquid chemical cleaning efforts,” he said. “Studies show that less than half the surfaces in a hospital room are properly disinfected after manual cleaning when the room is being prepared for the next patient.”
In 2020, COVID-19 stamped out years of steady decline in healthcare-associated infections and spurred increases in four of six routinely tracked infections. That achievement was the result of a perfect storm for antibiotic resistance and HAIs.
There were more and sicker patients during the global pandemic, and they required more frequent and longer use of catheters and ventilators. Those patient issues were coupled with staffing and supply challenges.
Beyond the problem of teams not being adequately armed with products necessary to protect healthcare facilities, there is the added challenge of staff shortages that can stretch existing employees too thin.
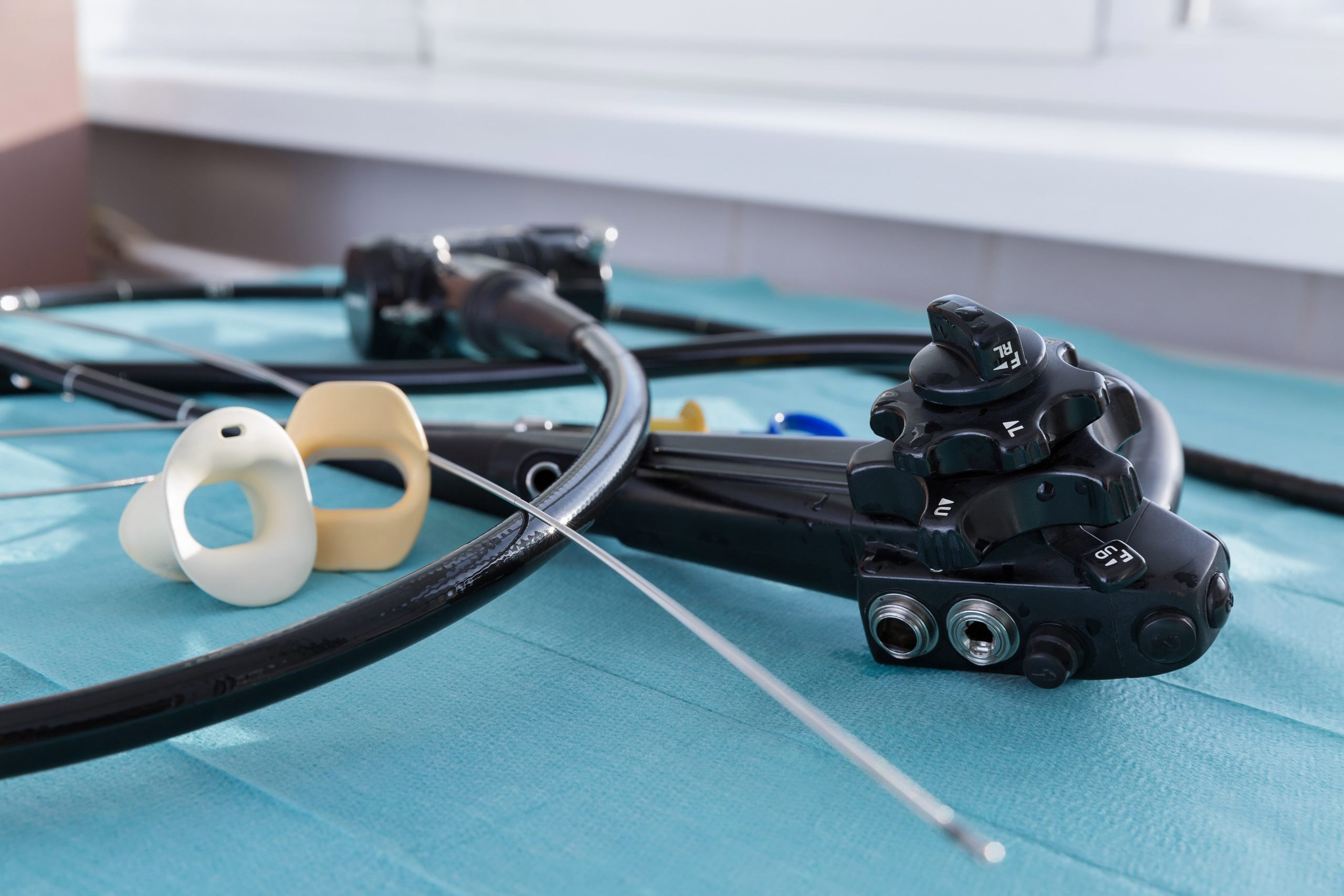
Single-use endoscope companies are touting the advantages that their devices offer as hospitals worldwide struggle with staffing shortages. Since single-use devices do not need to be reprocessed, they create more time for frontline clinical staff to focus on patients.
Lack of staff can result in bare-bones training, which in turn can breed ineffective cleaning and patient safety issues.
HAIs were among the 14 infection prevention topics of concern in a study recently published in The American Journal of Infection Control.
High-risk microorganisms like C.difficile, Candida auris and MRSA, which plague healthcare settings, are not going away anytime soon.
“So, the challenge is to do more with less,” Will Gerard, director of global marketing and product strategy at UltraViolet Devices Inc., told HPN.