A retrospective study at the New York University Langone Health Manhattan campus found that no healthcare workers contracted COVID-19 after using single-use endoscopes to perform bronchoscopy with intermittent apnea early in the global pandemic.
The research also identified bronchoalveolar lavage (BAL) as a more effective way to detect secondary infection with bacterial or fungal pneumonia among severely ill COVID-19 patents. The findings are detailed in “Safety and Efficacy of Bronchoscopy in Critically Ill Patients with Coronavirus Disease 2019,” published in CHEST in February 2021.
The research analyzed records from 412 patients with confirmed COVID-19 admitted to the hospital’s Manhattan ICU between March 13 and April 24, 2020. More than 300 of those patients required intubation. Approximately 33 percent of intubated patients underwent bronchoscopy.
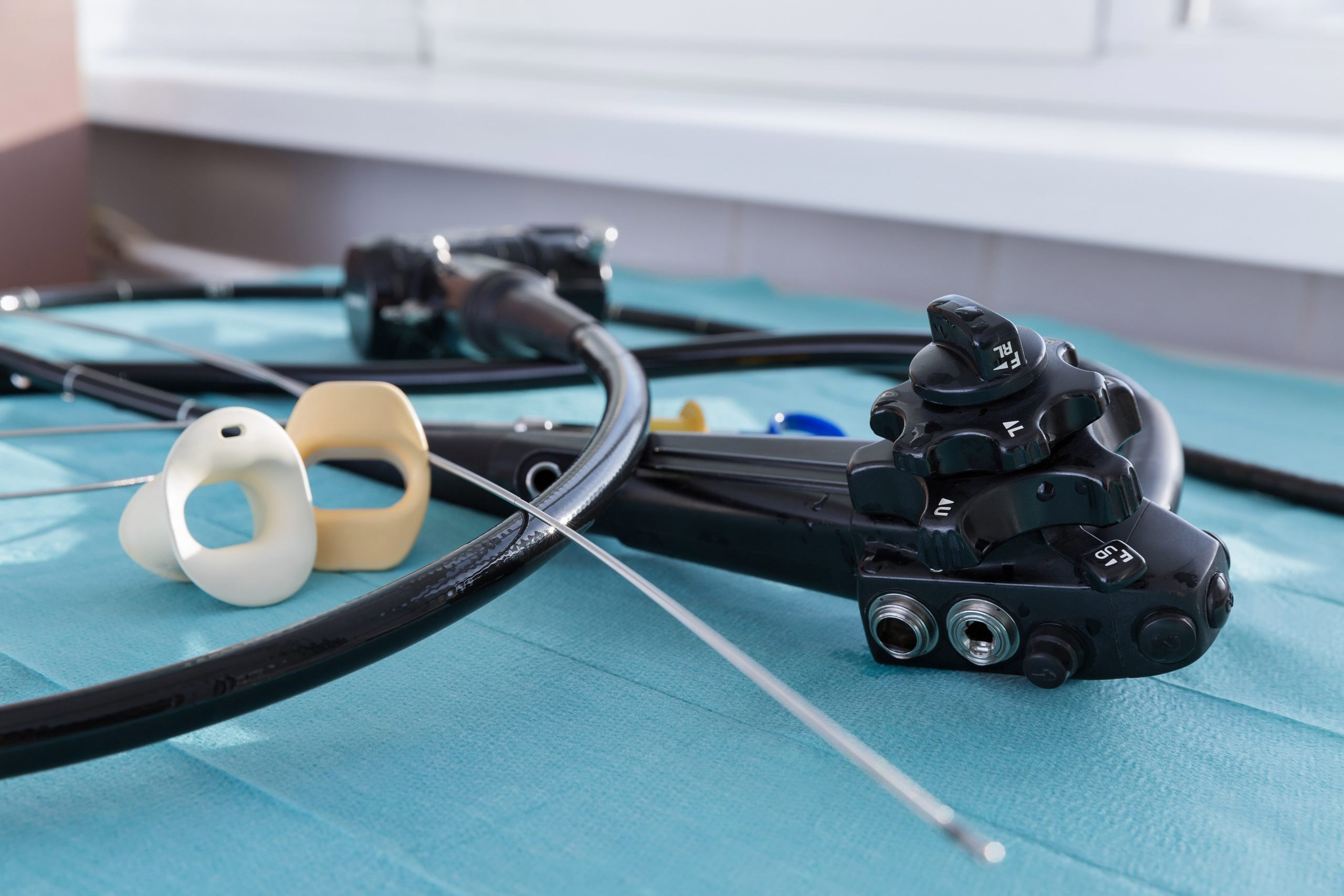
A total of 241 bronchoscopies were performed during the study period using Ambu single-use bronchoscopes and the Ambu® aView™ monitor, according to the review. Ambu A/S, a single-use endoscope manufacturer in Ballerup, Denmark, did not sponsor the study.
Disposable bronchoscopes have been recommended by many professional societies and international panels during the COVID-19 pandemic as a way to eliminate the risk of cross-contamination when bronchoscopy is deemed necessary.
“Because of concern regarding the safety of these procedures and possible high risk of transmission of COVID-19, many providers were reluctant to perform bronchoscopy,” the authors of the CHEST report write. “The protocol for neuromuscular blockade to decrease coughing and the performance of bronchoscopy under apnea was designed to minimize health-care provider exposure to COVID-19. ... No healthcare provider who was involved in the bronchoscopies became positive for COVID-19.”
All the procedures for this research were done in a negative pressure room with personnel wearing full personal protection equipment (hair cover, fitted N95 mask, face-shield, gown and gloves). The number of personnel inside the procedure room was kept to a minimum, with only the bronchoscopist inside and the bedside nurse available but outside the room, according to the review.
Patients who were not being sedated or receiving neuromuscular blockade were administered anesthesia, a procedure called bronchoscopy with intermittent apnea, to decrease the risk of spontaneous breathing that could lead to aerosolization.
The bronchoscopies were interrupted and patients were reconnected to a ventilator if oxygen saturation dipped below 90 percent. After further preoxygenation, the bronchoscopy was resumed.
None of the members of the hospital team was diagnosed with COVID-19 as a result of conducting the bronchoscopies. That team included six cardiothoracic surgeons and four cardiothoracic residents. One of the surgery residents had been found COVID-19-positive before performing any bronchoscopies.
The high rate of secondary infection identified in patients during the NYU Langone study is significant in better understanding the mortality rate, the authors write. What’s “more significant,” however, is how those secondary infections were identified, as nearly one-third of bronchoalveolar lavage samples confirmed secondary infection when tracheal aspirate cultures did not.
“These data directly contradict the belief that tracheal aspirate is sufficient for the diagnosis of superimposed pneumonias for patients with COVID-19,” the researchers write.
Dr. James M. Horowitz, medical director of NYU Langone Health’s Cardiac Care Unit, shared his experiences working in hard-hit New York City at the height of the pandemic in an Ambu-sponsored webinar last summer. Horowitz was not an author of this study.
In the webinar, Horowitz described the fear that swept the hospital initially and acknowledged that “bronching 100 percent disappeared,” at least for a time. As the weeks stretched on, he fought to save patients who were coughing severely and struggling to breathe through clogged airways. He and his team started performing bronchoscopies again using almost exclusively Ambu single-use bronchoscopes.