In response to the global COVID-19 pandemic, the Cleveland Clinic established a five-tier system to categorize the urgency of bronchoscopy procedures.
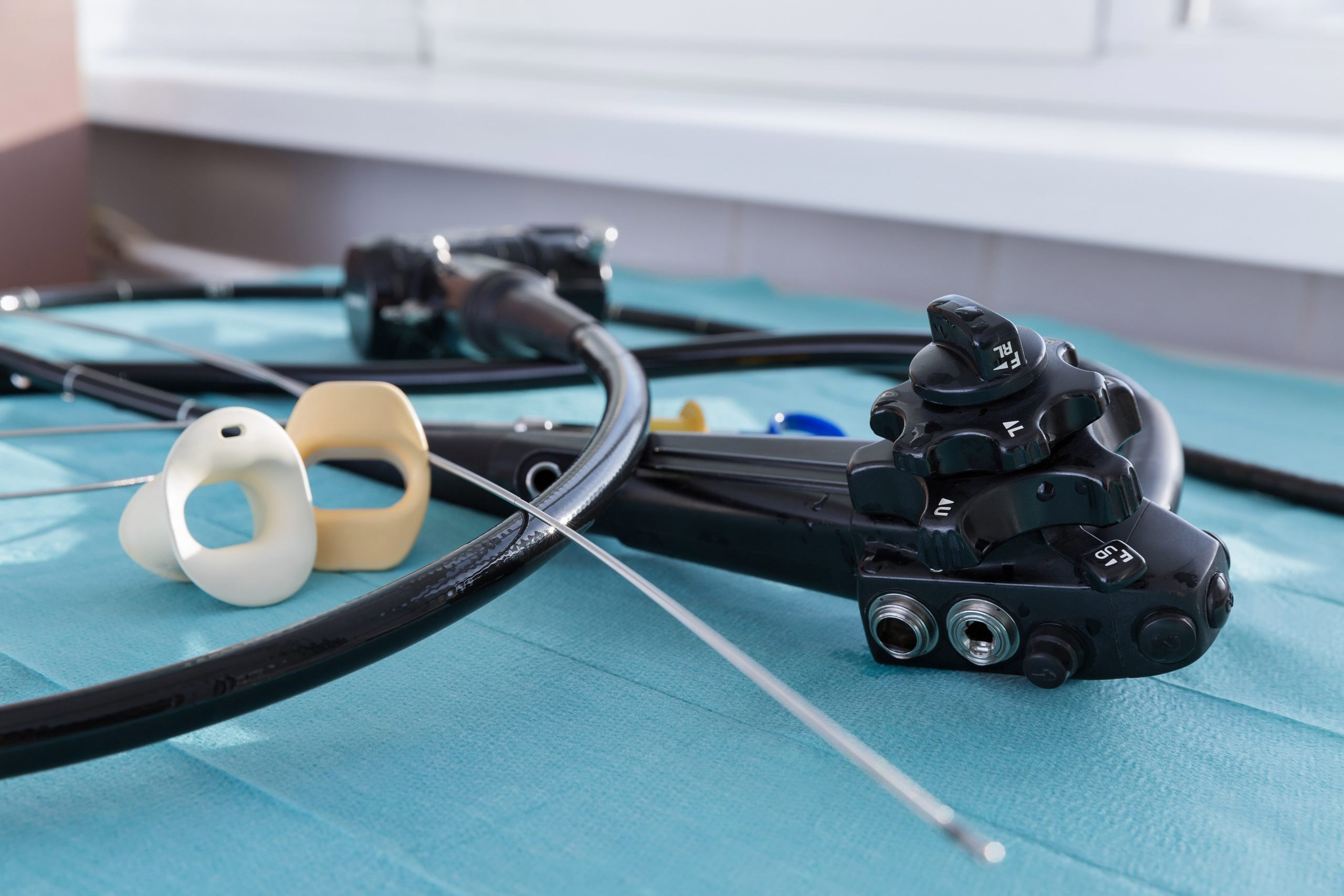
Bronchoscopy is challenging for healthcare workers because it’s an aerosol-generating procedure. It’s also used to diagnose and treat many diseases, so it was critical to have a plan in place to treat patients with or suspected of having the novel coronavirus.
The clinic’s tier system lays out each level of urgency for procedures and was detailed in research published in the Cleveland Clinic Journal of Medicine by Dr. Thomas R. Gildea and Dr. Basem B. Abdelmalak.
A central airway obstruction, critical tracheal stenosis, and tracheostomy complications were some of the procedures that should proceed the same day. Symptomatic bronchial stenosis, malignant airway obstruction, and advanced lung cancer diagnosis/staging were designated to be delayed a day or two.
Early stage lung cancer diagnosis/staging, routine stent change, and complex tracheostomy management were some of the procedures making up the urgent category. Reasons for semi-urgent bronchoscopy were lung transplant rejection follow-up, BAL for unresolving infiltrate, asthma “airway” evaluation, and tracheostomy tube change/revision.
Click here for the full list of procedures and where they fall among the five tiers. A similar tier system was published by the Society of Advanced Bronchoscopy.
“Infection control is intrinsic to the daily practice of bronchoscopy teams as they routinely manage respiratory pathogens including those requiring standard or contact precautions typical in hospital patients,” the authors write. “For example, droplet isolation is commonly used during seasonal viral infections, and respiratory isolation is needed for pathogens such as tuberculosis. Existing guidelines about personal protective equipment (PPE), room and space considerations, and various levels of isolation are core competencies.”
The most notable major change was for the use, reuse, and conservation of PPE. Strict protocols for donning and doffing of PPE were added. All healthcare workers wore N95 masks for the procedure rather than the surgical masks that had been previously worn.
Testing prior to bronchoscopy guides perioperative and postoperative care, the authors added. Patients who have not been tested for coronavirus are managed as if they are positive. The procedure takes place in the airborne infection isolation room, performed under general anesthesia administered intravenously.