Surgical masks and proper hand hygiene may sufficiently protect healthcare workers from COVID-19 during aerosol-generating procedures.
That’s according to a new case report that found 41 healthcare workers tested negative for the novel coronavirus after exposure to a COVID-19-positive patient during endotracheal intubation and laryngoscopy. Most of the healthcare workers wore surgical masks when in close proximity to the patient, while the remaining wore N95 masks.
Universal negative tests for all staff after a two-week home isolation period led case study authors to conclude surgical masks were enough to protect against COVID-19 during endotracheal intubation and laryngoscopy.
“Our observation is consistent with previous studies that have been unable to show that N95 masks were superior to surgical masks for preventing influenza infection in health care workers,” the report noted. “We emphasize, however, that nearly all experts recommend that health care workers wear an N95 mask or equivalent equipment while performing an aerosol-generating procedure.”
More on IIPW 2020:
Infection preventionists have played a vital role in protecting hospital staff and patients from COVID-19. That’s why the Association for Professionals in Infection Control and Epidemiology is calling attention to this work as part of this year’s International Infection Prevention Week.
While more research is needed, as the report’s authors note, it provides some insight into infection control measures needed to protect frontline healthcare staff during the novel coronavirus pandemic.
Healthcare workers are at risk of contracting the novel coronavirus by airborne transmission during procedures that generate aerosols, according to the World Health Organization. Airborne transmission refers to the presence of disease microbes that can remain in the air for long periods of time and be transmitted to others.
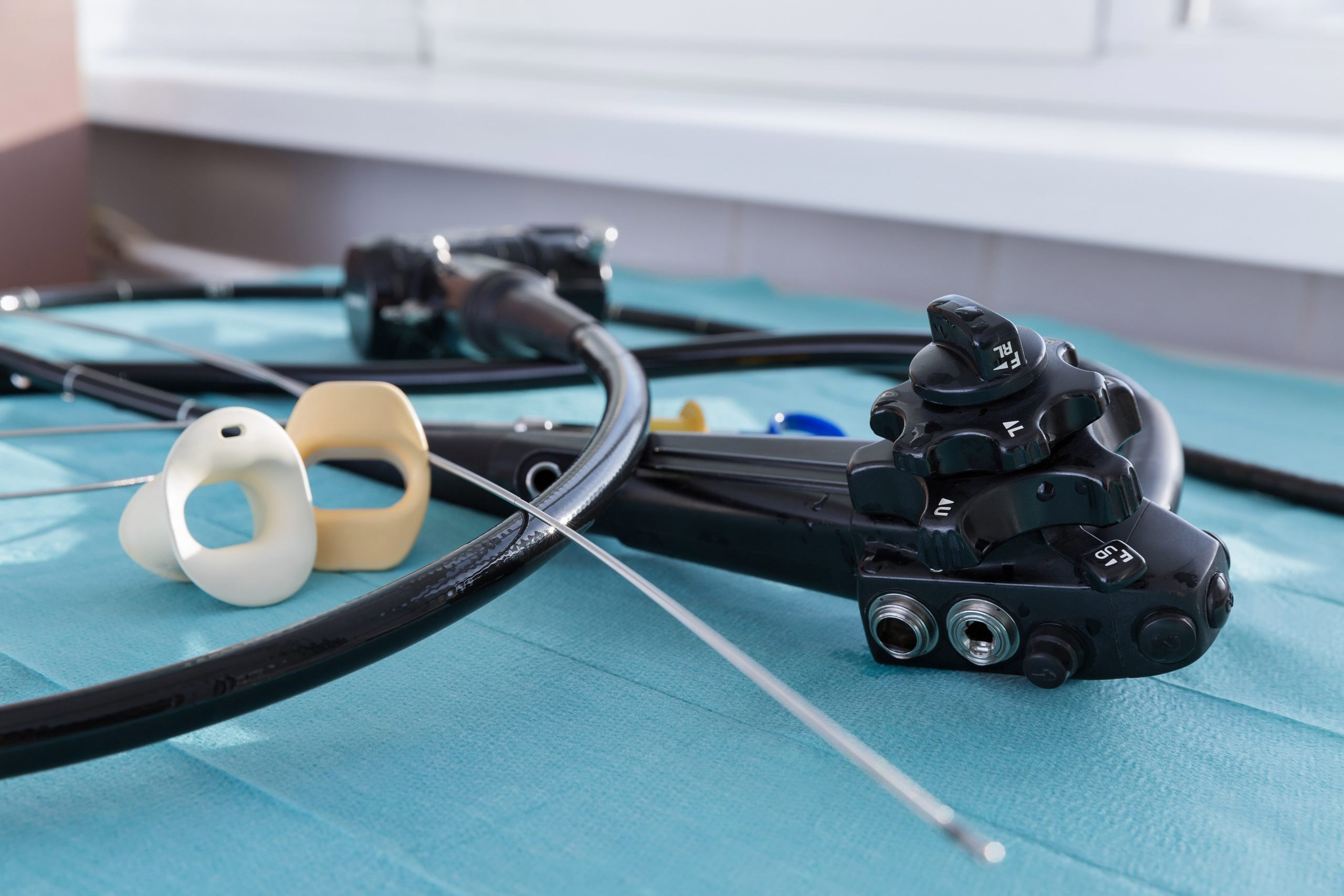
Back in March, as the virus was first spreading in the U.S., the American Association for Bronchology and Interventional Pulmonology said in new guidelines that if bronchoscopy was warranted during COVID-19 testing or treatment, physicians should use a disposable bronchoscope to protect patients and staff. Single-use bronchoscopes are intended for one-time use and do not require reprocessing, maintenance or repair.
All healthcare workers in this case report were within two meters (about 6.5 feet) of the patient for at least 10 minutes during the aerosol-generating procedures. The COVID-19 status of the patient was unknown at the time of treatment, according to the case report.
The Annals of Internal Medicine published “COVID-19 and the Risk to Health Care Workers: A Case Report” in June 2020.
The patient in question was hospitalized in February 2020 with community-acquired pneumonia. He reported no recent travel to China or any contact with anyone known to have COVID-19, according to the report.
After three days of treatment, he tested positive for the novel coronavirus. Through contact tracing, the hospital identified 41 healthcare workers who had close contact with the patient and were at risk.
All healthcare workers, regardless of wearing surgical masks or N95 masks, were tested regularly for two weeks following exposure. No workers reported developing any symptoms.